Prostatitis is inflammation of the prostate gland. It is one of the most common diseases in men. The majority of those affected are men over 30 years of age. If left untreated, the disease progresses rapidly and causes serious complications: infertility, impotence and cancer.
Most often, prostatitis manifests itself as pain during urination, purulent and bloody discharge in the urine, and sexual dysfunction.
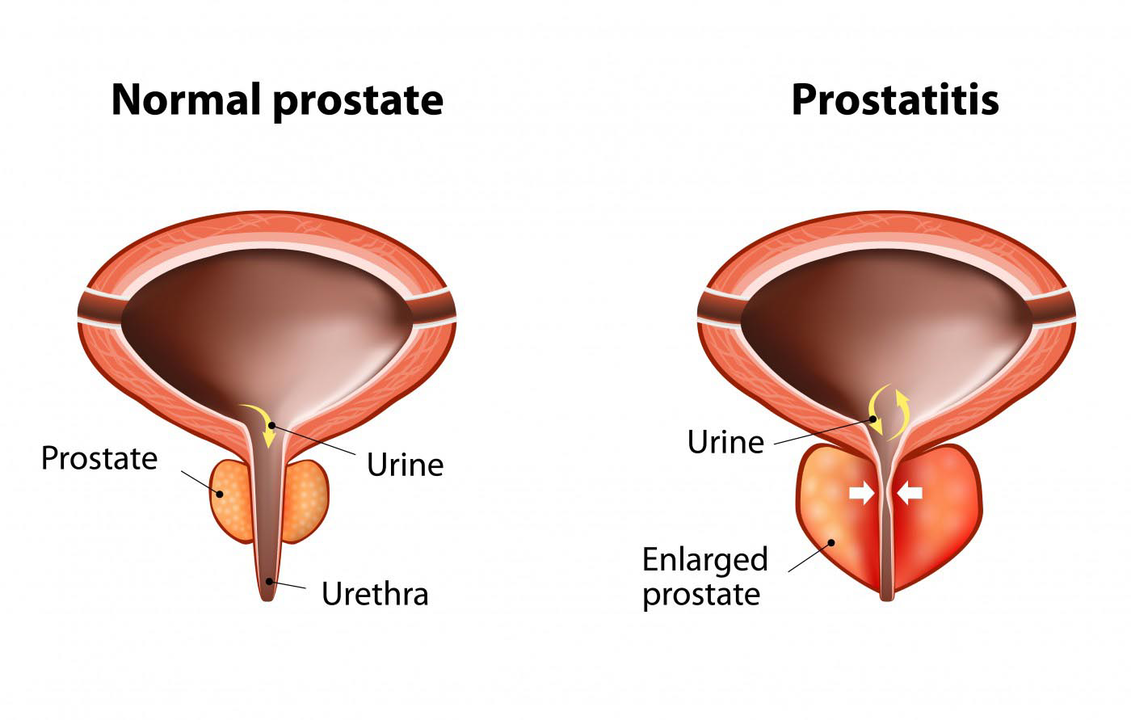
The prostate is the organ that produces sperm and regulates urination. It is located below the bladder. It consists of three departments. During ejaculation, the prostate begins to contract, pushing seminal fluid through the urinary canal. The gland participates in limiting urinary incontinence, in the formation of erection and in the production of sperm.
Prostate juice contains a large amount of proteins, fats, enzymes and even some vitamins. The juice dilutes the seminal fluid, thus promoting the viability of the sperm. The prostate is an active organ. It depends on hormonal levels and itself participates in the formation of sex hormones.
Causes
It is difficult to identify the exact cause that caused the development of prostatitis in a particular person. Most likely, it is a set of factors that, to one degree or another, caused the problem.
Let's consider the causes and factors that can contribute to the development of prostatitis:
- Hypothermia and stress. The body's defenses are reduced, which contributes to the appearance of inflammatory processes.
- Hormonal imbalances. The level of sex hormones affects the activity of the prostate gland.
- Sexually transmitted infections and urinary tract infections.
- Various disorders of the body's mechanisms: urination disorders, congestion in the pelvis. A hypodynamic lifestyle and tight underwear interfere with blood circulation in the pelvis. And problems with urination contribute to irritation of glandular tissue and cause prostatitis. Constipation can also be considered a predisposing factor.
- Prolonged abstinence from sexual relations, interrupted sexual relations or artificial prolongation of sexual relations. This leads to enlargement of the gland and its inflammation.
- Poor nutrition and alcohol abuse.
Infection in the prostate gland can occur in 4 ways:
- Descending: enters with the flow of urine.
- Ascending: rises along the urethra.
- Lymphogenic: along with lymph flow.
- Hematogen, along with blood flow.
Symptoms and signs of prostatitis.
Prostatitis symptoms can vary. Depending on the nature of the course, acute and chronic prostatitis are distinguished.
Common signs of prostatitis include the following:
- problems urinating: it is frequent, intermittent and difficult;
- deterioration of erection;
- burning sensation in the groin;
- the urine is cloudy and contains fibers;
- the orgasm is not brilliant;
- increased fatigue;
- decreased power;
- depression anxiety.
Acute prostatitis usually begins with an increase in body temperature of 39 to 40 degrees. The prostate gland swells and causes problems with urination. It is difficult and is accompanied by pain.
During an exacerbation of prostatitis, the patient experiences pain in the perineum, as well as in the rectum, groin and sacrum.
Acute prostatitis can be catarrhal, follicular and parenchymal. Characteristics of acute prostatitis:
- Acute follicular prostatitis is characterized by weak jet pressure during urination. It is accompanied by intense pain, which can radiate to the anal area, intensifying especially during defecation. A slight increase in temperature is possible.
- Acute parenchymal prostatitis is characterized by unexpected pain with pulsations in the perineal area. Intoxication of the body is observed, the temperature can reach 40 degrees. It is often accompanied by urinary retention.
- Acute catarrhal prostatitis causes pain in the perineum, frequent urination, and pain during urination.
Chronic prostatitis can develop from an acute form, but more often it immediately turns into a chronic form. The symptoms disappear, without clear signs or manifestations.
Symptoms and signs caused by chronic prostatitis:
- decreased erection and libido;
- decreased flow pressure when urinating;
- cramps and pain when urinating;
- aching pain in the perineum, anus, sacrum.
Since the signs of chronic prostatitis are not clearly pronounced, the patient often does not pay attention to the symptoms for a long time, which aggravates its development and can cause complications.
Diagnosis of prostatitis
Medicine does not stop and diagnosing prostatitis is not difficult. After collecting the anamnesis, the doctor may prescribe various diagnostic methods to confirm the diagnosis of prostatitis.
- Palpation of the prostate through the rectum to diagnose prostatitis. It will reveal pain and increase in size, and these are characteristic signs of the inflammatory process in it, and during palpation the secretion of the prostate gland is released, which is sent for analysis.
- Ultrasound examination.
- Microscopic examination of prostate secretion.
- Bacteriological examination of urine.
- A smear of mucous membranes and gland secretions to detect infection.
- Analysis of a smear from the urethra to determine sexually transmitted infections that can cause prostatitis.
- Blood test to determine sex hormones.

These diagnostic measures help not only to confirm the diagnosis, since in general the symptoms are quite pronounced, but also to identify the cause of the disease.
Prostatitis treatment
Currently, there are many treatment options for prostatitis. These include traditional methods and folk medicine methods. Traditional medicine can serve as a complement to basic therapy. It is dangerous to self-medicate prostatitis, as this can lead to complications.
Doctors always resort to the traditional medicinal method to treat prostatitis. This helps relieve swelling, severe inflammation and normalize the functioning of the prostate gland.
Usually a complex of several methods is prescribed:
- rectal suppositories. Reduce pain and relieve inflammation;
- injections;
- non-steroidal anti-inflammatory drugs;
- instillation - the drug is injected directly into the prostate;
- microenemas;
- medicines in tablets. Most often, antibacterial drugs;
- alpha blockers.
The set of therapeutic measures is selected individually, depending on the degree of the disease, the manifestation of symptoms and the expected therapeutic effect for the patient.
If a bacterial cause of prostatitis is identified, broad-spectrum antibiotics are prescribed that can destroy various strains of bacteria. They can be in the form of suppositories, tablets or injections.
Analgesics are used to relieve pain.
Alpha blockers help relax the muscles of the urethra, which is a consequence of prostatitis. Various muscle relaxants are used to relieve tension in the perineal area.
A necessary step would be to improve blood circulation to relieve congestion and take vitamins.
Various physiotherapeutic procedures and prostate massages are mandatory for the treatment of prostatitis. Prostate massage is used for all forms and stages of the development of the disease, it improves blood circulation and squeezes secretions with a pathogenic environment into the urethra.
Some scientists have become skeptical about this method of treating prostatitis, arguing that the pathogenic environment penetrates further into the genitourinary system and contributes to inflammation of other organs. Experiments are currently being carried out, this point of view has not been refuted or clinically proven, therefore massage is a comprehensive method of treating prostatitis.
Traditional treatment at home.
Traditional medicine is often used in the treatment of prostatitis at home. If chronic prostatitis is diagnosed, additional therapy with folk remedies will be of great help. It will not be superfluous in case of acute manifestation of prostatitis; however, home treatment alone is unacceptable.
Among the popular methods, the following can be considered quite effective:
- Treatment of prostatitis with pumpkin seeds. Pumpkin seeds contain a large amount of zinc, which is necessary for men, regardless of whether they have prostatitis.
- Treatment of prostatitis with parsley helps relieve inflammation and normalize sexual function. It contains a large amount of vitamins.
- Treatment of prostatitis with infusions of hemlock and celandine. This method should be used with caution, since these herbs are poisonous and strict adherence to the dosage and dosage regimen is necessary.
- Treatment of prostatitis with wormwood. It is used to relieve inflammation and eliminate purulent infection.
- Treatment of prostatitis with garlic, dill, hazelnuts, chestnuts, propolis, herbs, etc.
Most of these methods are aimed at relieving inflammatory processes and normalizing sexual function. A large number of different vitamins saturate the body, which plays a role in preventing exacerbations of prostatitis.
Consequences of prostatitis
If you refuse and if treatment for prostatitis is not started on time, there is a high probability of developing serious complications. Among the complications:
- sterility;
- impotence;
- HPB;
- prostate cancer and others.
If treatment is refused, the infection will penetrate further into nearby tissues. Other prostate diseases may also develop, including stones and cysts.
With prostatitis, the level of sex hormones decreases, which leads to a decrease in sexual desire (libido). Erectile dysfunction begins and premature ejaculation may occur. Helplessness is possible.
Prostatitis also leads to infertility. This problem is especially common in those patients who have developed chronic prostatitis. This complication is observed in half of these patients.
Sclerosis of the prostate gland may develop. In this case, the gland partially or completely stops working. This problem is accompanied by severe pain, sexual dysfunction, and problems urinating.
Prostate adenoma and prostate cancer are the most dangerous complications of prostatitis.
The problems and complications that prostatitis entails, in one way or another, affect a man's sexual life. This leads to psychological problems, stress and depression.
It is important to carefully monitor the signs in order to recognize chronic prostatitis in time.
Prostatitis prevention
Prevention of exacerbations is aimed at monitoring health and timely identification of problems. Since in most cases prostatitis is a consequence of untreated diseases of the genitourinary system, close attention should be paid to the treatment of such diseases.
Prostatitis is considered a disease that is easier to prevent than to cure.
Of the preventive methods, the most important are:
- Sport activities. They serve to improve blood circulation in the pelvis, prevent the appearance of congestion and strengthen the pelvic muscles.
- Normal sexual life. Medications to artificially prolong sexual intercourse, interrupt sexual intercourse and suppress ejaculation are undesirable.
- Rejection of promiscuity. Violent sex life leads to sexually transmitted infections.
- Proper and healthy nutrition.
- Give up alcohol.
- Strengthening the body's defenses, avoiding hypothermia.
- Minimize stress.
Prostatitis has a low rate of self-cure or home treatment. Therefore, at the first signs, you should immediately contact a urologist to prescribe appropriate treatment. It is also necessary to carefully monitor signs indicating chronic prostatitis and consult a doctor in time.































